On May 20, 2025, the Food and Drug Administration announced a new stance on who should receive the COVID-19 vaccine.
The agency said it would approve new versions of the vaccine only for adults 65 years of age and older as well as for people with one or more risk factors for severe COVID-19 outcomes. These risk factors include medical conditions such as asthma, cancer, chronic kidney disease, heart disease and diabetes.
However, healthy younger adults and children who fall outside of these groups may not be eligible to receive the COVID-19 shot this fall. Vaccine manufacturers will have to conduct clinical trials to demonstrate that the vaccine benefits low-risk groups.
FDA Commissioner Marty Makary and the agency’s head of vaccines, Vinay Prasad, described the new framework in an article published in the New England Journal of Medicine and in a public webcast.
The Conversation U.S. asked Libby Richards, a nursing professor involved in public health promotion, to explain why the changes were made and what they mean for the general public.
Why did the FDA diverge from past practice?
Until the May 20 announcement, getting a yearly COVID-19 vaccine was recommended for everyone ages 6 months and older, regardless of their health risk.
According to Makary and Prasad, the Food and Drug Administration is moving away from these universal recommendations and instead taking a risk-based approach based on its interpretation of public health trends – specifically, the declining COVID-19 booster uptake, a lack of strong evidence that repeated boosters improve health outcomes for healthy people and the fact that natural immunity from past COVID-19 infections is widespread.
The FDA states it wants to ensure the vaccine is backed by solid clinical trial data, especially for low-risk groups.
Was this a controversial decision or a clear consensus?
The FDA’s decision to adopt a risk-based framework for the COVID-19 vaccine aligns with the expected recommendations from the Advisory Committee on Immunization Practices, an advisory group of vaccine experts offering expert guidance to the Centers for Disease Control and Prevention on vaccine policy, which is scheduled to meet in June 2025. But while this advisory committee was also expected to recommend allowing low-risk people to get annual COVID-19 vaccines if they want to, the FDA’s policy will likely make that difficult.
Although the FDA states that its new policy aims to promote greater transparency and evidenced-based decision-making, the change is controversial – in part because it circumvents the usual process for evaluating vaccine recommendations. The FDA is enacting this policy change by limiting its approval of the vaccine to high-risk groups, and it is doing so without any new data supporting its decision. Usually, however, the FDA broadly approves a vaccine based on whether it is safe and effective, and decisions on who should be eligible to receive it are left to the CDC, which receives research-based guidance from the Advisory Committee on Immunization Practices.
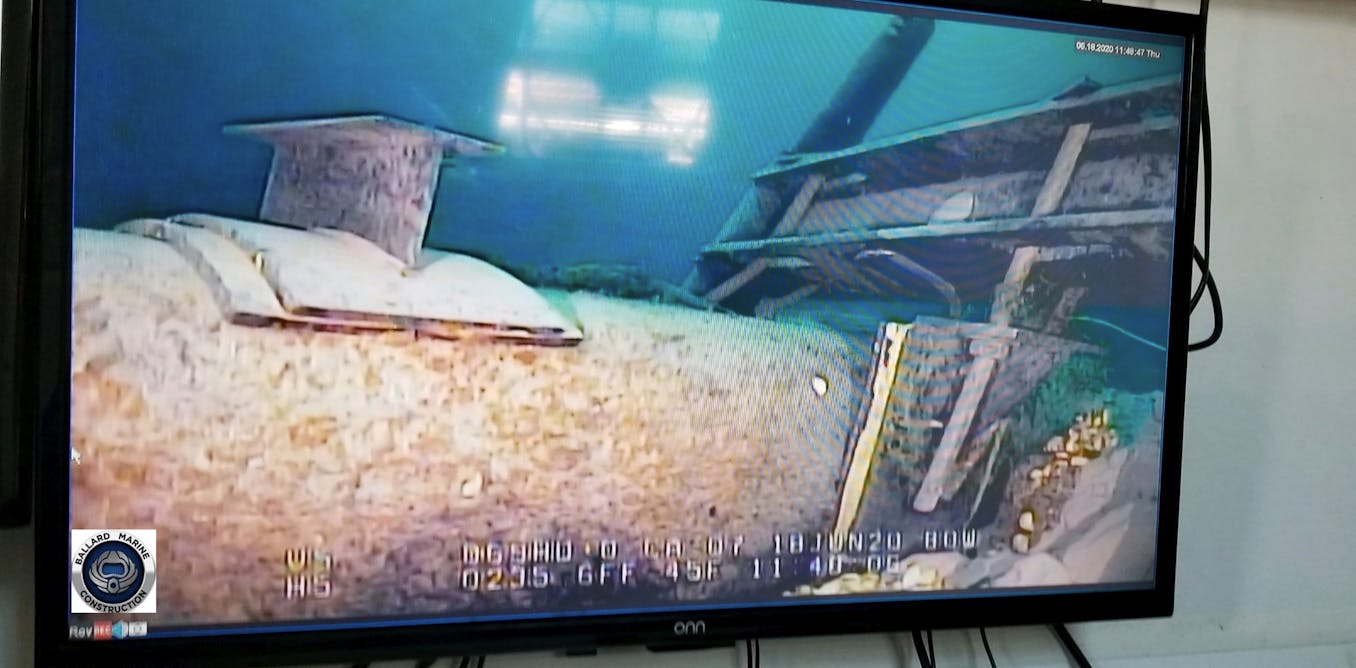
Rock Obst, CC BY-SA
Additionally, FDA officials point to Canada, Australia and some European countries that limit vaccine recommendations to older adults and other high-risk people as a model for its revised framework. But vaccine strategies vary widely, and this more conservative approach has not necessarily proven superior. Also, those countries have universal health care systems and have a track record of more equitable access to COVID-19 care and better COVID-19 outcomes.
Another question is how health officials’ positions on COVID-19 vaccines affect public perception. Makary and Prasad noted that COVID-19 vaccination campaigns may have actually eroded public trust in vaccination. But some vaccine experts have expressed concerns that limiting COVID-19 vaccine access might further fuel vaccine hesitancy because any barrier to vaccine access can reduce uptake and hinder efforts to achieve widespread immunity.
What conditions count as risk factors?
The New England Journal of Medicine article includes a lengthy list of conditions that increase the risk of severe COVID-19 and notes that about 100 million to 200 million people will fall into this category and will thus be eligible to get the vaccine.
Pregnancy is included. Some items on the list, however, are unclear. For example, the list includes asthma, but the data that asthma is a risk factor for severe COVID-19 is scant.
Also on the list is physical inactivity, which likely applies to a vast swath of Americans and is difficult to define. Studies have found links between regular physical activity and reduced risk of severe COVID-19 infection, but it’s unclear how health care providers will define and measure physical inactivity when assessing a patient’s eligibility for COVID-19 vaccines.
Most importantly, the list leaves out an important group – caregivers and household members of people at high risk of severe illness from COVID-19 infection. This omission leaves high-risk people more vulnerable to exposure to COVID-19 from healthy people they regularly interact with. Multiple countries the new framework refers to do include this group.
Why is the FDA requiring new clinical trials?
According to the FDA, the benefits of multiple doses of COVID-19 vaccines for healthy adults are currently unproven. It’s true that studies beyond the fourth vaccine dose are scarce. However, multiple studies have demonstrated that the vaccine is effective at preventing the risk of severe COVID-19 infection, hospitalization and death in low-risk adults and children. Receiving multiple doses of COVID-19 vaccines has also been shown to reduce the risk of long COVID.
The FDA is requiring vaccine manufactures to conduct additional large randomized clinical trials to further evaluate the safety and effectiveness of COVID-19 boosters for healthy adults and children. These trials will primarily test whether the vaccines prevent symptomatic infections, and secondarily whether they prevent hospitalization and death. Such trials are more complex, costly and time-consuming than the more common approach of testing for immunological response.
This requirement will likely delay both the timeliness and the availability of COVID-19 vaccine boosters and slow public health decision-making.
Will low-risk people be able to get a COVID-19 shot?
Not automatically. Under the new FDA framework, healthy adults who wish to receive the fall COVID-19 vaccine will face obstacles. Health care providers can administer vaccines “off-label”, but insurance coverage is widely based on FDA recommendations. The new, narrower FDA approval will likely reduce both access to COVID-19 vaccines for the general public and insurance coverage for COVID-19 vaccines.
The FDA’s focus on individual risks and benefits may overlook broader public health benefits. Communities with higher vaccination rates have fewer opportunities to spread the virus.
What about vaccines for children?
High-risk children age 6 months and older who have conditions that increase the risk of severe COVID-19 are still eligible for the vaccine under the new framework. As of now, healthy children age 6 months and older without underlying medical conditions will not have routine access to COVID-19 vaccines until further clinical trial data is available.
Existing vaccines already on the market will remain available, but it is unclear how long they will stay authorized and how the change will affect childhood vaccination overall.

The post “FDA limits access to COVID-19 vaccine to older adults and other high-risk groups – a public health expert explains the new rules” by Libby Richards, Professor of Nursing, Purdue University was published on 05/21/2025 by theconversation.com


































Leave a Reply