When Harrison Chow and Boris Heifets met up at a burger joint in Palo Alto in 2019 to talk about dreams, Heifets balked a little at what he was hearing. A giant hotdog chasing a man through San Francisco’s financial district? Blue Corvettes driving in endless loops around gas stations in Silicon Valley? Firefighters bow-hunting in Mexico? Like the intricately weird details of a psychedelic trip, tales of elaborate dreams usually just put listeners to sleep, interesting only to the dreamer herself.
But these weren’t just any dreams — they were hyper-vivid, anesthesia-induced dreams that Chow’s surgical patients had been reporting to him over the past decade, and they seemed to be helping these people heal.
“I am generally skeptical,” Heifets, a neuroscientist and assistant professor of anesthesiology at Stanford Medical School, tells me. “It’s served me well to be skeptical of anything I hear.”
But what Chow served up next blew his mind a little. Heifets, who studies psychedelics, had been wrestling with a question — one that he thought only applied to psychedelics: What makes them therapeutic for some people? Is it the expectation of feeling better? The biochemical effects of the drug? The subjective experience of the trip? He’d been leaning toward focusing on experience — perhaps the therapeutic value of psychedelics lies not in the drugs themselves but in the subjective state they produce.
Chow, a Stanford-trained anesthesiologist and medical doctor, launched into a story about an orthopedic patient who had come in with a chronic foot problem. She had also happened to have been diagnosed with agoraphobia. After dreaming under anesthetics, her PTSD symptoms seemed to improve.
“What he was describing to me — dreams induced by anesthetics — was so similar to what I’d been wondering about psychedelics,” Heifets says. “It fit with this idea that it doesn’t matter what the drug is; it’s the state. If you just induce a state where people can re-live prior experiences, project their priors onto the large blank screen of their dreams, work through trauma, whatever…” then you have a shot at a therapeutic effect.
The patient, who lived alone in a small house with a German shepherd, had dreamt during surgery that she escaped the sexual abuse she’d experienced as a child. The dream seemed to transform a nightmare into a happy ending, and she woke up feeling well. Not only that, but her foot appeared to be healed in the dream. She reverted to her old agoraphobic routine after a few days, Chow said, but the anesthesia-induced dream seemed to have conferred a big enough effect to help her leave the house and go to Starbucks. The anesthetic agent used was propofol, the most common induction agent for general anesthesia. But interestingly, Chow told Heifets he’d seen the same effect using various types of anesthetic drugs for different surgeries.
And it wasn’t just the odd patient here and there — it was hundreds.
Anesthesia dreams
Anesthesia dreams have likely been a common phenomenon since surgeons first started putting patients under in the 1840s, but there has never been sound reason to study, let alone prolong, them. In fact, early published reports of anesthesia dreams frame them as pesky side effects of an otherwise smooth medical procedure. Regarded as a mysterious feature of the brain, there was little reason to suspect that, under certain conditions, these dreams might have therapeutic value.
“Most anesthesiologists blow right past this,” Heifets says, adding that they pass off dreaming as a meaningless byproduct of surgery or wake up patients before they fall deeply enough into the dream state.
But the phenomenon piqued Chow’s interest. Since 2009, he’s collected observational data on many elaborate anesthesia dreams that seemed to help people manage anxieties that had nothing to do with the surgery itself.
Hearing the story of the woman resolving her abuse in one such dream, Heifets’ ears perked up.
“I’ve been very involved with MDMA both on the clinical and basic science side, and that’s the story that people tell: being able to touch the experience in a way that was far less traumatic.”
Heifets agreed to set Chow up with an EEG monitor and a team to do psychiatric evaluations and formalize the observations Chow had been collecting over the years. Finishing their burgers and clinking their beers, the two were off to the races.
Into the dream world
This wasn’t the first time Chow and Heifets had crossed paths. Heifets had started as a resident at Stanford in 2010, when Chow was a clinical instructor. “I fondly remember Boris [Heifets] as a resident,” Chow tells me.
Chow, who grew up in nearby Saratoga and graduated from Stanford Medical School in the 1990s, recently left a 20-year career in private practice to return to Stanford. He couldn’t help spreading the word about what he was seeing.
Around 2009, he started noticing patterns in his orthopedic and cancer patients. “People were dreaming about things that made them happy — especially in orthopedic situations, about things that seemed to be relieving their anxiety.”
First, there was Minivan Mom, who went in for breast cancer surgery and dreamt of overcoming the anxiety of getting her kids to school on time, driving them to school in a minivan “on time” for days in a perpetual state of punctuality. After the operation, she beamed at Chow: “I got my kids to school on time!” Then there was Corvette Man, who came in for hand surgery and dreamt of driving the beloved blue Corvette he’d anxiously sold years back, in a repeated loop around the 76 gas station in his town.
And finally, there was Déjà vu Man, a loan agent who had anxiety over all the backed-up loan applications he needed to process at work. His anesthesia dream was abruptly interrupted; he explosively woke up during his hernia surgery thinking there were “strangers in his office” (OR staff). The patient said he’d been processing files on his desk during the dream. When Chow called him for a follow-up days later, the man reported an odd experience upon returning to the office: He felt that he’d already processed the backed-up applications, in a déjà vu-like fashion that seemingly could only be explained by having “gone through the motions” during his anesthesia dream. The details of the applications were irrelevant; he just had a strong feeling that he’d already done what he was about to do.
But it wasn’t until a young man working in finance came in for a simple surgery that Chow started taking things more seriously. Before the operation, he mentioned to Chow that he was anxious about feeling hungry going into surgery. Chow didn’t think much of it. When the man woke up, he reported dreaming that he’d been chased by a giant hotdog down Market Street near his office in downtown San Francisco. When the hotdog finally caught him, wrapping him in its colossal buns, he woke up and said, “I feel great. I’m not hungry anymore.” It was like he’d projected his emotions onto the hotdog, Chow said. It didn’t last, as his hunger quickly returned, but for 20 or 30 minutes, “there was this clinical effect where his brain was being tricked into something else.”
Chow had already gathered some insights from the work of Australian researcher and anesthesiologist Kate Leslie, who characterized anesthesia dreams as “unstructured” and “random.” But that’s where Chow disagreed.
In his post-surgical observations, he’d found by chance that if he extended the dream state, patients experienced less postoperative nausea and vomiting, recovered more quickly, were unusually alert and conscious and ready to leave the OR, often claimed to have awoken from the “best sleep of their life,” and were discharged earlier from the post-anesthesia care unit.
But most intriguing of all the observations was that patients reported structured, non-random, and movie-like dreams with a beginning, middle, and end. He observed three dream types: perpetual (Minivan Mom), looping (Corvette Man), and interrupted (Déjà Vu Man). The content usually involved resolving emotional issues, most frequently anxiety, in hyper-vivid detail. Like turning a radio dial of consciousness to the right frequency, he seemed to have stumbled upon a sweet spot other clinicians hadn’t noticed.
Something else distinguished the dreams, which neither Leslie nor other anesthesia dream researchers had noted: Patients also dreamt of resolving physical issues, sometimes alongside emotional issues.
In 2021, a flurry of Chow’s patients started showing the same pattern. A hand surgery patient dreams of throwing dice at the Bellagio in Las Vegas with a repaired hand. Another hand surgery patient dreams of riding her motorcycle across the desert, where she broke her wrist before. An ankle surgery patient dreams she can walk and play with her grandchildren again. A wrist surgery patient dreams her wrist is healed and now she can shop for Thanksgiving dinner supplies at Safeway.
The pattern continued into 2022: One hand surgery patient, a local fire chief, dreams of completing a fire abatement plan for the city and travels to Mexico to bow-hunt with a healed wrist. Another hand surgery patient, himself a cardiac surgeon, dreams of preparing for a surgical procedure with his own hand repaired. An ankle surgery patient dreams of dancing in Santa Monica with her old boyfriend, while another hand surgery patient, an ex-Olympian hammer thrower, dreams of throwing again with a healed hand. (The Olympian, by the way, asks to be left alone to continue the dream.)
At the time, Chow didn’t think to ask these patients whether they’d also dreamt of emotional repair, but he didn’t have to, because that’s when the moms started showing up.
First, two moms from Palo Alto came in for breast cancer surgery and left having reunited with their dead sons in highly vivid and emotional dreams.
Mare Lucas, who had a right-breast lumpectomy in 2020, tells me that even though everyone uses the word “dream” for this phenomenon, hers could more accurately be described as an experience.
“I’m floating above the room where our youngest son was born,” she says. “I can see him in the bassinet. I can hear the older children’s voices. I’m not watching him be born. I’m watching the joy of his birth.”
In a dream you are acting, you are first-person, she says. “This isn’t first-person. This is hovering above, and just sucking in the joy and the beauty.”
Lucas, who suffered from PTSD and weekly nightmares for three years after her eldest son’s suicide in 2017, has not had nightmares since that first surgery in 2020. A year after her experience, she no longer met the criteria for PTSD. On the verge of tears, Lucas tells me she was so affected by the experience that she believes her son might still be alive today if he’d had access to the treatment himself.
Another mom, Kelsey Newman, dreamt of being with her eight-year-old son — dreamt that he was safe.
Newman, a schoolteacher whom Chow treated on four different breast cancer mastectomy surgeries over three years, starting in 2021, says the dream study was transformative. Leading up to each of her four surgeries, she was terrified of the operation and “going under.” That is, until she started dreaming.
“I started looking forward to what I was going to dream about,” Newman told me. “I became curious instead of freaked out. Each dream I had offered some solace and gave me comfort that I was going to be okay.”
“The fourth surgery and last dream study I had with Dr. Harrison Chow had the biggest impact on me because it resolved the breast cancer I had been fighting.”
In the dream, she finished her book and traveled around Europe with her son on a book tour, cancer-free. She woke up calm and felt assured that everything would be alright.
“Even though I have hoops to go through now and am still dealing with healing my body of cancer,” she told me, “I can see the light at the end of the tunnel and that last dream gave me hope, like a future-telling prophecy that all will be well.”
By this point, the “dream team” had split into two fully operational teams, one consisting of clinical providers headed by Chow and one clinical research team headed by Heifets. On Chow’s side, a protocol had been perfected for surgical patients with the help of Miranda Shull, CRNA. Over on the Heifets side, team members were developing protocols for healthy volunteers.

It was around this time that Marina came to them. Marina, 26, had been attacked by a family member at close range with a knife and needed reconstructive surgery for her right hand. While she didn’t meet the criteria for lifetime PTSD, she had symptoms, including a recurring nightmare that kept her from sleeping or doing much of anything for two weeks before she got to the OR, where Chow took care of her. Under surgical anesthesia, she dreamt of being attacked with a knife in her apartment, going to the emergency room, proceeding to the OR for surgical repair, looking at her repaired hand, and returning home and completing errands with her healed hand. Afterward, she was able to calmly speak about the attack, stopped having nightmares, and no longer met the criteria for acute stress disorder.
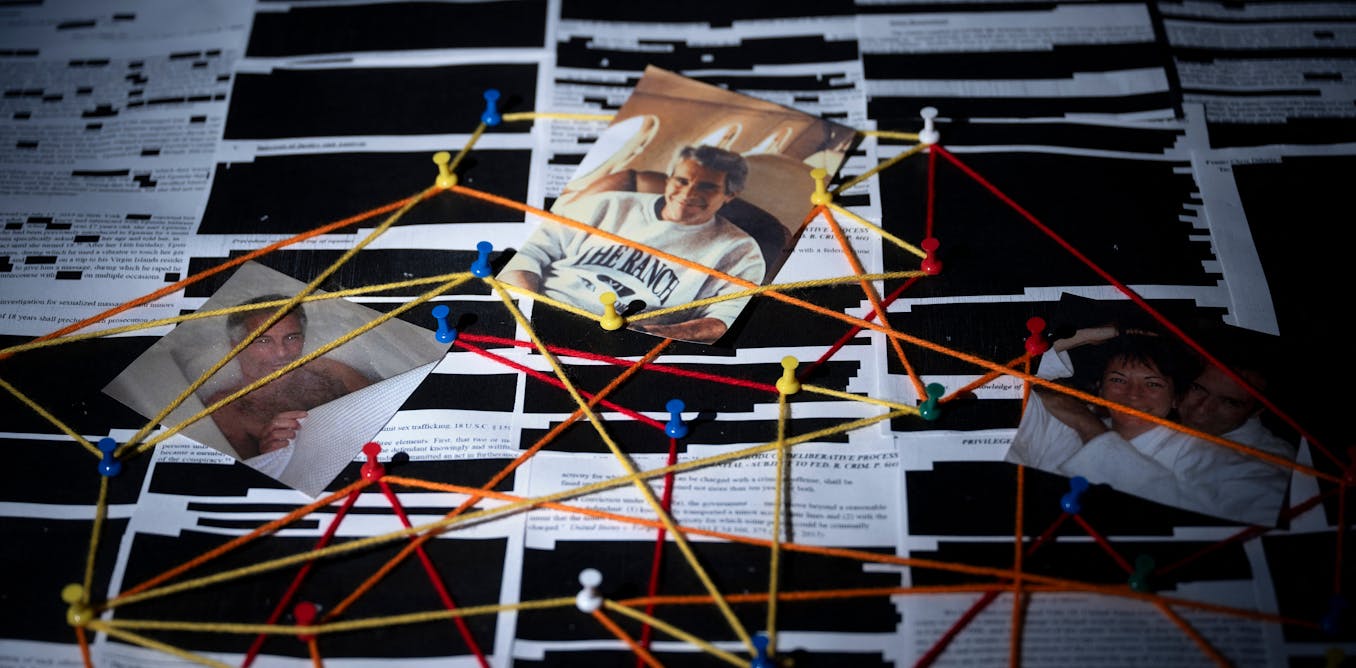
Heifets picked up on the fact that, like Newman, the patient had had the same dream four times. They created a term for this: “looping.” The team “caught everything on film” with EEG and published the results in their first case study.
The remarkable thing, to Heifets, was how similar this “dream therapy,” as they’d started calling it, was to a commonly used psychotherapy for PTSD: exposure therapy. Prolonged exposure therapy helps patients reduce their emotional responses to traumatic memories through habituation and extinction. Over about a dozen 90-minute sessions, a trained therapist guides the patient in safely revisiting their trauma through imaginal exposure. “It’s exposure-based: How can you get people to recall a memory in a way that’s safe and keeps them from shutting down or hyper-activating?”
When Marina shared her report, Heifets thought it was “a truly wild narrative.”
“Exactly the script you would expect for exposure therapy for PTSD or imagery rehearsal therapy — all of it.” He was flabbergasted. “How can you ignore this parallel?”
Even so, the team is in the beginning stages of testing whether anesthesia dreams do in fact have clinical, therapeutic value. They began in the OR in different patient populations. Now they’re moving outside the OR, which has excited their research colleagues at Stanford and elsewhere.
“The baton goes to Boris now to turn a bunch of observations over 15 years into some form of science so that we can treat patients,” Chow says. “I’m on the other end of Boris’s lab, waiting for the product to come out so that we can actually treat patients.”
Disconnecting consciousness
Heifets has been interested in the intersection of psychiatry and anesthesia for many years, with expertise in running psychiatric trials in anesthetic-type settings like the OR. Much of his work has focused on ketamine, an anesthetic that has been repurposed as a psychiatric agent. But he’s worked with MDMA, psilocybin, and other psychedelic drugs. What’s been interesting, in comparing all these agents, is how similar they are as a “new therapeutic class” (compared to SSRIs, for example, which are very different and still represent the gold standard in the pharmacological treatment of stress disorders), and yet how vastly unrelated their action is in the brain.
What links drugs like psilocybin, MDMA, ketamine, and really any experiential therapy (unlike SRRIs) is three things: they’re psychoactive, rapid-acting, and durable.
“One of the things that struck me, after doing this work for 15 years, is that they all have the same pattern of [points just mentioned] but no similarity in pharmacology. When you start using receptors to explain how these things work, it unravels immediately.”
The way Heifets has been thinking about it — and where Chow’s work fits in, incidentally — is that the aim of his research, at this point, is to try to deconstruct the psychedelic experience: What is it about these transformational events that can lead to long-term therapeutic benefits? There’s the set and setting, the drug effect, and the trip. Trying to separate the drug and the trip has enormous consequences for how drugs and therapeutics are developed in the US and worldwide, he says.
“A focus on biochemistry irrespective of experience… that’s the model we’re used to. That’s what SSRIs do.”
There have been efforts to engineer psychedelics to be non-hallucinogenic, where “we’ll just encode resilience into every dendrite of your brain and that’ll be the therapy.” Maybe it’ll work, he says, but that’s an empirical question that needs to be tested. The Heifets Lab is collaborating with a lab at UC Davis to do just that.

One way of testing this is to “blank the experience.” For example, if people attribute the therapeutic effect of ketamine to the intensity of the dissociative psychedelic experience, what happens if you give it during anesthesia? “There is no experience; there’s just the drug.”
The flip side: What if you could generate a psychedelic-like experience without a psychedelic drug at all? Ultimately, his lab is trying to determine whether it’s the expectation, biochemical effect, or experience that’s potentially therapeutic.
That’s where anesthesia dreams come in.
“I think you can see the crossover between psychedelic medicine and dream therapy, and all the issues combined. This really feels like experiential medicine. It centers the role of human experience in transformation and mental health recovery — much more than drug-based solutions.”
Chow echoes: “It’s not really a propofol thing; it’s a brain-state thing.”
But how does experiential medicine work exactly? No one knows. During a team meeting, where the researchers sat around offering possible explanations, psychiatrist Makoto Kawai speculated that dreams at a cellular level may cause selective cerebral neuron exhaustion of norepinephrine (a neurotransmitter that responds to stressors in the environment).
“That just kind of fit with what you see,” Chow said. “Basically, these patients have something anxious. They have this dream in surgery and they just stop caring about it. They feel really good about it.”
Heifets offered that dreaming may be an “epiphenomenon” (a byproduct of brain activity) stemming from an intrinsic neurological process rather than a standalone phenomenon. The bottom line is that if this is a truly unique state that clinicians and patients can access through anesthesia-induced dreaming, then our understanding of it is wide open.
“We currently have no objective way to detect consciousness or its specific contents,” Dr. Pilleriin Sikka, a postdoc at the Heifets Lab with an impressive background in dream research, told me when I visited the lab in person. “Until such methods exist, subjective reports are our primary tool. We take these reports as valid and work to identify the neural or biological markers associated with the experiences people describe.”
As we chatted in the cozy room of the lab, I noticed a simple reclining chair between us with a neatly folded drape and pillow on its seat, ready for the next round of dreamers.
If anesthesia-induced dreams prove to have a transformative impact, she said, it will indicate not only neurobiological changes “but also — or perhaps, specifically — shifts in how individuals perceive and interpret the world and themselves.”
Again, the Stanford Dream Team is by no means the first to study anesthesia-induced dreams. There is an 80-year history of people reporting dreaming during anesthesia, where patients lose consciousness during surgery but retain some memory of dream content upon waking. There’s even a practice called “narcosynthesis,” where patients are given anesthetic drugs in psychiatric settings with the goal of disinhibition to elicit emotional content.
That’s not what this is, Heifets says.
“We’re talking about disconnected consciousness,” he says emphatically. “We’ve made it a more precise thing. It’s clearly internally generated. [The state] is between general anesthesia, which can be tracked with an EEG, and connected consciousness, where you’re awake and connected with the external environment.”
The researchers don’t know exactly where or what defines it, and Heifets says that EEG is not quite sufficient to describe it, since EEG is heavily biased toward activity on the surface of the brain and it’s “not just stuff going on in the cortex; there’s a lot of subcortical things happening.”
Sikka adds that the team is in conversation with researchers who study epilepsy, using transcranial stimulation, to see if their methodology could be of use.
That said, it’s more about designing a good intervention at this point than describing what’s happening at the neurological level.
“We’re using EEG, but to say that we know how it works is a little early,” Heifets says. “It’s enough to do a trial. We don’t need to know how it works to help people get better.” To know more about mechanisms will require calling in neurosurgeons, imagers, people putting electrodes in various parts of the brain. “That’s how I see the evolution of this.”
Is it propofol? Sure, Heifets concedes, but it depends on how you do it. No one is cured by a dose of propofol any more than they are by a dose of MDMA. People have been using propofol for decades and aren’t spontaneously remitting from all their problems. “It’s really about the state.”
The art of medicine
After publishing several research articles on top of Marina’s case study, including a case report in the American Journal of Psychiatry and a journal article in Sleep, the team secured funding from the Tiny Blue Dot Foundation to develop the phenomenon into a well-characterized intervention that can be tested in PTSD, framed as a psychiatric trial. They have started a more comprehensive screen, systematically capturing this phenomenon. The IDEA lab, run by Heifets, Sikka, and resident Ben Deverret, will kick off a three-year experimental trial starting in early 2025.
It’s very unusual, Sikka tells me, referring to Chow and Heifets’ collaboration and how this research came about. “This never happens,” she says, noting the puzzling yet persistent divide between the medical field and brain science. “They don’t really talk to each other.”
But the way Chow and Heifets relate to each other is clearly part of why this whole thing works. They correct each other’s mistakes without reservation at least as often as they commend each other’s work. Chow is the narrator, weaving together details and centering human experience. Heifets is the critic, careful to bring in skepticism when needed. In an email thread between the three of us, Chow dives into a detailed answer to my question, only to be curbed by Heifets:
“I have no doubt the patients you take care of have excellent outcomes. I still would be careful about claiming this technique or style of doing anesthesia has perfect outcomes. Some people may believe you, but scientists will not and you will lose credibility.”
In nearly the same breath, Heifets says of Chow’s work, “It’s really the art of medicine,” making a detailed clinical observation and fine-tuning the protocol around it. That valuable slice of the dream world can go by in the blink of an eye, he says, so extending it is truly innovative. “Harrison has trained the OR to shut up when patients are waking up. ‘Don’t touch the patient; give the patient space.’ Really creating a therapeutic environment.”
Along with Sikka and the rest of the Dream Team, they are now focused on doing the work, going back and forth between basic science and clinical research, to get this treatment to clinics. “If we have a positive trial, which is not a foregone conclusion,” Heifets says, “then we go the FDA route. We can do it off-label. You’ll see it spread quickly. The amount of interest is enormous. People are dropping in and coming out of the woodwork, trying to understand how to do this.”
This article Inside the emerging world of anesthesia “dream therapy” is featured on Big Think.

The post “Inside the emerging world of anesthesia “dream therapy”” by Saga Briggs was published on 01/21/2025 by bigthink.com


































Leave a Reply